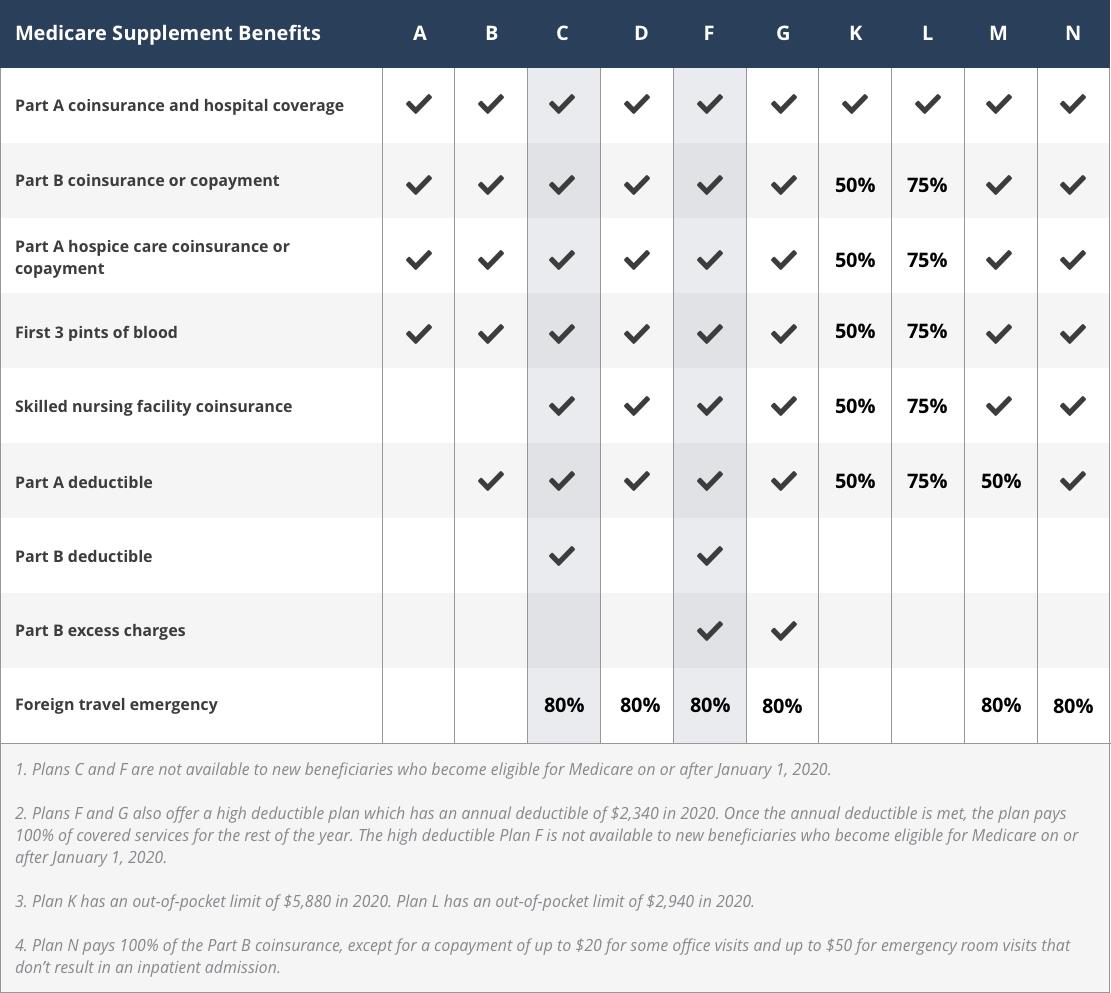
ORIGINAL MEDICARE "DEDUCTIBLE" IS DETERMINED BY THE UNITED STATES
GOVERNMENT on an annual basis
The annual
deductible
for all Medicare Part B beneficiaries is $226 in
2023
Plan A - Hospital Coverage
Plan B - Office vistits and non-hospital visits (x-rays, tests,
etc).
Meaning that some hospital procedures may be included
in Part B and not Part A
Plan C - is NOT ORIGINAL MEDICARE.
Plan C is also ONLY available for people who because eligible on, or
before, January 1, 2020
Plan D - ALL pharaceutical plans that ARE SUPPLEMENTAL to ORIGINAL
MEDICARE
Plan F - IS NOT available for people who because eligible on, or
before, January 1, 2020. Plan F covers everything - including coverage for
annual deductible.
HOWEVER, if you became eligible before 2020, you may be able to enroll in
Plans F or C as long as they are available in your area.
Plan G - Pays 100% of EVERYTHING not covered by Plans A&B
AFTER the annual deductible is met/paid
Plans F and G
offer a HIGH DEDUCTIBLE option of $2700 per year (the deductible is set by the US Government on an annual
basis). Once deductible is paid, 100% of covered expenses are paid
Plans F and G are the ONLY Medigap Plans that pay Excess
Charges (Charges "allowed" by Original Medicare, but OVER acceptable)
Plan K - has an out-of-pocket yearly limit of $6940 (this
limit is set by the US Goverment on an annual basis). After the $6,940 is
paid, insurance pays everything at 100% for the calendar year
Plan L - has an out-of-pocket yearly limit of $3,470 (this
limit is set by the US Goverment on an annual basis). After the $3,470 is
paid, insurance pays everything at 100% for the calendar year
Plan M -
Deducibles and ALL excess charges are the
responsibility of the patient
Plan N-
Pays 100% of Part B coinsurance, except for a
copayment of up to $20 for some office visits and up to $50 copayment for
emergency room visits that are so not result in an inpatient admission
________________________________________________________________________
Cost of Medigap plans vary, depending on the company that is selling the
plans AND depending on what area the patient lives in.
If a person moves,
they have to "re-do" Medigap AND Advantage coverage to "meet" the new
location.
Medicare guides and availabilities. Massachusetts, Minnesota and Wisconsin have different Medigap standards
There are 9 standardized benefits included in
consideration of purchase of Medigap Plans:
-
Medicare Part A coinsurance and hospital costs
Medicare Part A covers hospital costs IF patient is admitted to
a hospital for inpatient treatment, after you reach the Medicare Part A
deductible of $1600 per year.
Patients are not require to pay the Part A coinsurance of $1600 for
the first 60 days of a hospital stay
HOWEVER, on day 61 of the hospital stay, Patients are required to pay
"Medicare Part A coinsurance" at a cost of
$400
per day through day 90.
After 90 days in the hospital, patients must pay
$800
per day for up to 60 more days. After a total of 210
days in the hospital Medicare no longer covers, and a patient becomes
responsible for all hospital costs.
-
Medicare Part A deductible
Before your Part A coverage kicks in, you are required to pay
the Part A deductible ONLY IF a patient has a hospital stay of more than
60 days. The Medicare Part A deductible isn't an annual deductible -
this deductible is PER hospitalization. This means that you could
potentially have to meet the Part A deductible more than once in a given
year.
-
Medicare Part B deductible
Before Medicare Part B covers any of your costs for things like
doctor's appointments, x-rays, tests, medical devices, etc., a patient
has to pay the annual deductible. $226 in 2023. The US Government sets a
new deductible each year.
-
Medicare Part B coinsurance or copayment
After Part B deductible is met, a patient is required to pay a copay of
20% of Medicare-approved amounts for your COVERED
SERVICES. There is no limit to how much you may be required to pay for
this 20 percent copayment or coinsurance in a given year, if you do not
have a Medigap plan that provides coverage for this cost.(MAKE SURE that
your doctor, clinic, hospital is CONTRACTED to accept Medicare!!!!!
-
Medicare Part A hospice care coinsurance or copayments
If a patient receives hospice care that is covered by Medicare,
you are required to pay a Part A copayment for prescription drugs you
use during hospice. You may also be charged 5 percent coinsurance for
inpatient respite care costs.
-
Coinsurance for skilled nursing facility
There is no coinsurance requirement for the first 20 days of
inpatient skilled nursing facility care. However, a
$200 per day
coinsurance requirement begins on day 21 of your stay, and you are then
responsible for all costs after day 101 of inpatient skilled nursing
facility care (in 2023).
-
Medicare Part B excess charges
Excess charges can be accrued when a
patient receives Medicare-covered services or items from a provider who
is not contracted with Medicare. This means that a provider may not
accept Medicare payment as full payment for their services. In this
case, the provider can reserve the right to charge the patient up to 15%
more than the Medicare-approved payment.
-
First three pints of blood
Original Medicare does not provide coverage for the first three
pints of blood that are used in a blood transfusion.
-
Foreign travel emergency care
Medicare does not typically provide coverage for emergency care
received outside of the U.S. or U.S. territories.